Researchers from the Hebrew University have succeeded in isolating a variant of the Newcastle Disease Virus (NDV-HUJ), which usually affects birds, in order to specifically target cancer cells. The research, which has already cleared the first phase of clinical trials, is already patented and if all goes well it might receive an approval for clinical use, changing the way we think about viruses forever.
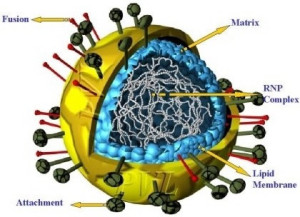
Professors Amos Panet and Zichria Zakay-Rones, from the Department of Virology at the Hebrew University Hadassah Medical School, have been involved during the past five years in research that could create a new and effective weapon in the fight against cancer, as well as change the way we look at viruses. As an obligatory parasitic entity with no independent life of its own, a virus must enter a living cell in order to multiply. The viral life-cycle begins when the virus inserts its genetic material into the hosts cell, forcing it to replicate the virus components, and eventually leading to the death of the cell. The NDV-HUJ virus, discovered by the Hebrew University in Jerusalem team, acts in a similar way, except for its outstanding preference for infecting cancerous cells. NDV-HUJ is a natural variant of NDV (Newcastle Disease Virus) which usually affects birds. Being an attenuated variant (e.g., weakened virus), it is innately preferentially targets and replicates in certain types of tumor cells, leaving normal cells almost unaffected.

A plausible (though not yet proved) explanation suggested by the researchers for this interesting behavior might be linked to some deficiencies of the Interferon-system inside cancerous cells. Interferon is a natural anti-viral substance which serves as the bodys first line of defense against viruses. As opposed to the activation of the immune system and antibodies production, the Interferon system is activated immediately after the infection process has taken place, and acts to diminish the viral replication. Thus, deficiencies in this system make the cancerous cells more vulnerable to viral infections such as the NDV-HUJ. Chemotherapy, the current main weapon against cancer is non-selectively effective against proliferating cells and thus is severely harmful to healthy tissues, such as the hair, skin, digestive and immune systems. Using the NDV-HUJ virus will enable doctors to specifically target cancer cells without the risk of severely affecting the patient.
Viro-therapy History
Viro-therapy is not a new idea. Its roots could be found in the mid 20th Century, when a number of physicians noticed an interesting phenomenon: some of their patients, who suffered from cancer and had an incidental viral infection, or subjected to vaccination, were now improving, experiencing a remission from their symptoms. In the 40s and 50s, studies were conducted in animal models to evaluate the use of viruses in the treatment of tumors, and in 1956, one of the first human clinical trials with an oncolytic virus (“onco” meaning cancer, “lytic” meaning “killing”) was conducted in patients with advanced-stage cervical cancer. Nevertheless, systematic research of this field was delayed for years, due to lack of more advanced technologies. In recent years the research in the field of oncolytic viruses began to move forward more quickly. Last year it was reported that researchers from the Ohio State University Medical Center have been trying to use a genetically engineered herpes virus against one type of brain tumor in mice. The Ohio State researchers have modified one of the herpes genes so it will be active only in cells that made a protein called nestin. The results of the mice research were encouraging and some of the mice who received the treatment lived a few days more than the control group who did not receive the treatment.
The Hebrew University NDV-HUJ research:
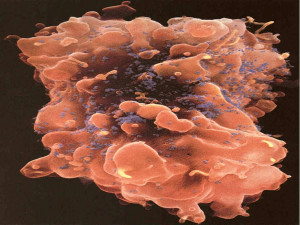
The first stage of the research conducted at the Hebrew University focused on mapping the NDV-HUJ genome (which has 6 genes and 15,068 nucleotides), comparing it to other strains of the NDV virus and analyzing the differences. The next stage of the research focused on the way the NDV-HUJ causes a process known as apoptosis. Apoptosis or “programmed cell death” is the end stage in the life cycle of a cell. Every form of existing cancer treatment is aimed at causing selective apoptosis of cancer cells. The problem is that in cancer cells the apoptosis mechanism is damaged, thus allowing the cells to exist beyond their normal life span and multiply out of control. Existing cancer treatments use the apoptosis mechanism to destroy cancer cells, but due to the damage done to its apoptosis mechanism the cancer cell requires a stronger treatment in order to activate its “self destruct” mechanism. Stronger treatments mean more damage to normal cells in the body which is why Chemotherapy is considered such a harsh treatment.
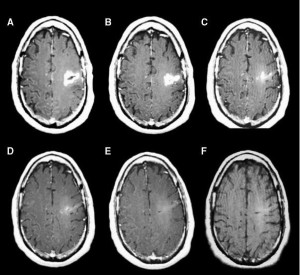
The first stage of clinical trials conducted at the Hadassah Medical Center between December 2002 and December 2003 involved 14 patients suffering from Glioblastoma Multiforme, (GBM), an aggressive type of primary brain tumor, accounting for 52 percent of all primary brain tumors cases. Until now treatment for GBM involved chemotherapy, radiotherapy and surgery. The aggressive nature of the cancer lead to the fact that the five-year survival rate of the disease has remained unchanged over the past 30 years, and stands at less than three percent. After receiving the NDV-HUJ virus treatment, one of the 14 patients exhibited a regression of the tumor, a surprising fact given the aggressive nature of the GBM cancer and the early phase of the clinical trials. These initial results are encouraging since no adverse side effects were noticed in the treated individuals. To understand why this is the case we need to look at the three main advantages of the NDV-HUJ virus over existing forms of cancer treatment, including some of the existing viro-therapy concepts:
- Like the rest of the Newcastle Disease Virus strains, the NDV-HUJ is a bird virus, and unlike the Herpes virus and other potential oncolytic viruses it is not considered pathogenic to humans. This is important for two main reasons: first, the virus meets relatively low resistance from the patients immune system which can otherwise reduce the effectiveness of the treatment. The second reason has to do with the fact that being a bird virus, the NDV-HUJ has a very low risk of a mutation that will cause it to become dangerous to humans. Furthermore, being an RNA virus it would not integrate into cell DNA genome.
- The ability of the NDV-HUJ to specifically target cancer cells is exceptionally high and therefore toxicity of the virus to normal tissues is minimal.
- The NDV-HUJ virus used in the clinical trial is an attenuated strain which does not pose any danger to birds even if it will somehow infect them.
Further research is being carried out on the NDV-HUJ mechanisms of action, and more advanced clinical trials should be performed in the near future, and the researchers are optimistic that within the next few years the field of oncolytic viruses will be able to give cancer patients new hope for recovery.

In order to accelerate the development of the new virus-based treatment the Hebrew University technology transfer company Yissum and the Hadassah Medical Center technology transfer company Hadasit, have helped the research team fund a new start-up company by the name of TheraVir. In an interview with IsraCast, Professor Panet explained that at the present time the team continues to research the NDV-HUJ virus in order to better understand the way it works and to try and discover whether it will be possible to use the virus against other kinds of cancer (in the laboratory the virus was also shown to be effective against Lymphoma and lung cancer). This part of the research is being carried out with funds from the Philip-Morris international fund. As for the clinical research, there are currently preparations being made for more advanced studies.Professor Panet added that part of the costs associated with the development of the new NDV-HUJ treatment could be cut by using the existing facilities that produce standard vaccines for other viruses.
More on cancer reaserch from Israel:




